What can I take for hot flushes? This question plagues countless individuals seeking relief from the discomfort and disruption caused by these sudden, intense episodes of heat. Hot flashes, a common symptom of menopause and other hormonal imbalances, can significantly impact quality of life.
In this comprehensive guide, we delve into the causes, remedies, and strategies for managing hot flashes, empowering you with the knowledge and tools to regain control and comfort.
From lifestyle modifications and over-the-counter solutions to prescription medications and alternative therapies, we explore a wide range of options to address the unique needs of each individual. Join us on this journey as we unravel the complexities of hot flashes and discover effective remedies for lasting relief.
Hot Flushes Overview
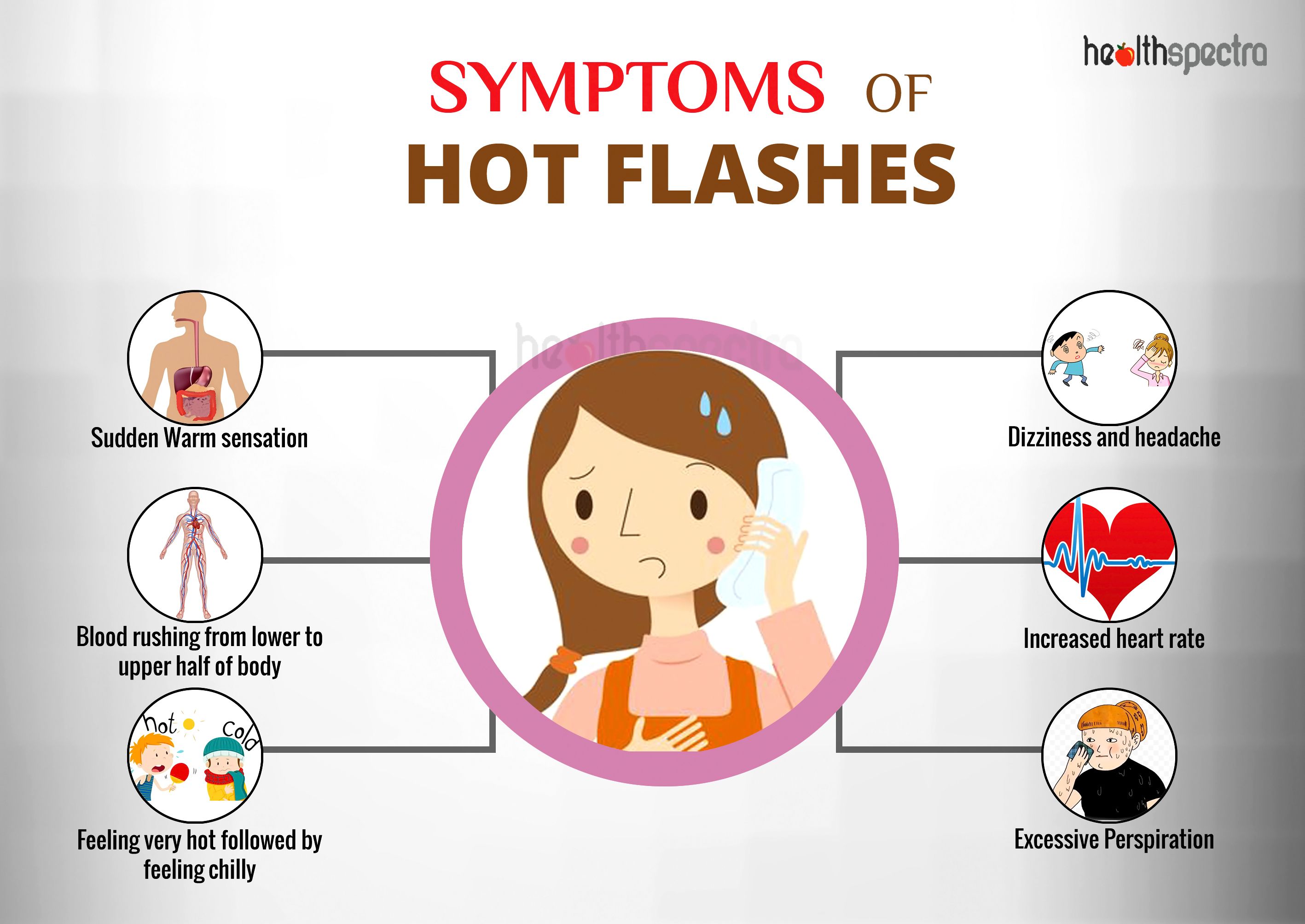
Hot flushes, also known as vasomotor symptoms, are a common experience for many individuals, particularly during the menopausal transition and beyond. These episodes are characterized by a sudden feeling of intense heat and sweating, often accompanied by a rapid heart rate and facial flushing.
Hot flushes can be triggered by various factors, including hormonal changes, certain medications, and lifestyle habits.
Physiologically, hot flushes occur due to a disruption in the body’s thermoregulatory mechanisms. During menopause, declining levels of estrogen can lead to instability in the hypothalamus, the brain region responsible for regulating body temperature. This instability can cause the body to misinterpret normal body temperature fluctuations as being too high, triggering a compensatory response to cool down.
Hot flushes can significantly impact quality of life, affecting sleep, mood, and daily activities. They can cause discomfort, embarrassment, and interfere with social interactions. In severe cases, hot flushes can lead to anxiety, depression, and reduced productivity.
Lifestyle Modifications
Lifestyle modifications can play a significant role in managing hot flushes. These include dietary changes, stress management techniques, and regular exercise.
Adopting these modifications can help alleviate the intensity and frequency of hot flushes, improving overall well-being during menopause.
Dietary Changes
Dietary modifications can help reduce hot flushes by addressing underlying triggers. Some recommendations include:
- Reducing caffeine and alcohol intake: These substances can trigger vasodilation, leading to hot flushes.
- Limiting spicy foods: Capsaicin, a compound found in spicy foods, can stimulate the release of heat-producing hormones.
- Avoiding sugary foods: Sugary foods can cause blood sugar spikes, which can trigger hot flushes.
- Increasing soy intake: Soy contains isoflavones, which have estrogen-like effects and may help reduce hot flushes.
- Eating cooling foods: Foods such as cucumbers, watermelon, and mint can help cool the body and reduce hot flushes.
Stress Management
Stress can exacerbate hot flushes. Managing stress levels can help reduce their frequency and intensity.
- Practicing relaxation techniques: Yoga, meditation, and deep breathing exercises can help calm the nervous system and reduce stress.
- Getting enough sleep: Sleep deprivation can increase stress levels and worsen hot flushes.
- Engaging in enjoyable activities: Spending time with loved ones, pursuing hobbies, or reading can help reduce stress and improve overall well-being.
Regular Exercise
Regular exercise has numerous benefits for menopausal women, including reducing hot flushes.
- Improving circulation: Exercise can improve blood flow, which helps regulate body temperature.
- Relieving stress: Exercise releases endorphins, which have mood-boosting and stress-reducing effects.
- Building muscle mass: Muscle mass helps regulate body temperature, reducing the risk of hot flushes.
Over-the-Counter Remedies
Over-the-counter medications can provide temporary relief from hot flushes. However, it is important to consult a healthcare professional before taking any medications, as some may have side effects or interact with other medications you are taking.
Commonly used over-the-counter remedies for hot flushes include:
Supplements
Several supplements have been studied for their effectiveness in reducing hot flushes. These include:
- Black cohosh: A plant-based supplement that has been shown to reduce the frequency and severity of hot flushes in some women. However, it may interact with certain medications, such as blood thinners and hormone replacement therapy.
- Red clover: Another plant-based supplement that contains isoflavones, which are compounds that have estrogen-like effects. Red clover may help to reduce hot flushes, but it is important to note that it may also interact with certain medications, such as blood thinners and hormone replacement therapy.
- Evening primrose oil: A plant-based supplement that contains gamma-linolenic acid (GLA), which is an essential fatty acid that may help to reduce hot flushes. However, it is important to note that evening primrose oil may interact with certain medications, such as blood thinners and anticonvulsants.
Other Medications
Other over-the-counter medications that may help to reduce hot flushes include:
- Ibuprofen: A non-steroidal anti-inflammatory drug (NSAID) that can help to reduce the severity of hot flushes. However, it is important to note that NSAIDs can have side effects, such as stomach upset and bleeding.
- Acetaminophen: A pain reliever that can help to reduce the discomfort of hot flushes. However, it is important to note that acetaminophen can be toxic to the liver if taken in high doses.
It is important to note that the effectiveness of over-the-counter remedies for hot flushes can vary from person to person. Some women may find that one remedy is more effective than another. It is also important to be aware of the potential side effects of any medication you are taking, and to talk to your healthcare professional if you have any concerns.
Prescription Medications

Prescription medications are an option for women who experience severe hot flashes that significantly interfere with their daily lives. These medications work by regulating hormone levels or blocking the effects of hormones that trigger hot flashes.
The effectiveness of prescription medications for hot flashes varies depending on the individual and the type of medication used. Some women may experience complete relief from hot flashes, while others may only experience a reduction in the severity or frequency of hot flashes.
Hormone Replacement Therapy (HRT)
HRT is a type of medication that replaces the hormones that are lost during menopause. These hormones include estrogen and progesterone. HRT can be taken in the form of pills, patches, or gels.
HRT is effective in reducing hot flashes in most women. However, HRT is not recommended for women who have a history of breast cancer, blood clots, or liver disease.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are a type of antidepressant that is also effective in reducing hot flashes. SSRIs work by increasing the levels of serotonin in the brain. Serotonin is a neurotransmitter that is involved in mood regulation.
SSRIs are generally well-tolerated, but they can cause side effects such as nausea, dizziness, and insomnia.
Clonidine
Clonidine is a blood pressure medication that is also effective in reducing hot flashes. Clonidine works by blocking the effects of norepinephrine, a hormone that is involved in the regulation of body temperature.
Clonidine is generally well-tolerated, but it can cause side effects such as dry mouth, constipation, and dizziness.
Alternative Therapies
Alternative therapies offer a holistic approach to managing hot flushes, focusing on improving overall well-being and reducing the severity of symptoms. These therapies include herbal remedies, supplements, acupuncture, acupressure, mindfulness, and relaxation techniques.
While scientific evidence for the effectiveness of alternative therapies varies, many women have reported positive results. It’s important to discuss these options with your healthcare provider to determine the most suitable approach for your individual needs.
Herbal Remedies and Supplements
Certain herbs and supplements may provide relief from hot flushes by reducing inflammation, balancing hormones, or promoting relaxation. Common herbal remedies include black cohosh, red clover, and ginseng. Some studies have shown that these herbs may reduce hot flush frequency and severity, but more research is needed to confirm their long-term effectiveness.
Supplements such as vitamin E, vitamin B6, and magnesium have also been suggested as potential remedies for hot flushes. However, it’s important to consult with a healthcare professional before taking any supplements, as they may interact with other medications or have potential side effects.
Acupuncture and Acupressure
Acupuncture and acupressure are traditional Chinese medicine techniques that involve stimulating specific points on the body to promote healing. Acupuncture uses fine needles, while acupressure applies pressure using the fingers or a blunt object.
Some studies suggest that acupuncture and acupressure may help reduce hot flush frequency and severity. These therapies aim to balance the body’s energy flow, which is believed to play a role in regulating body temperature.
Mindfulness and Relaxation Techniques
Mindfulness and relaxation techniques can help manage stress, which is a common trigger for hot flushes. Techniques such as deep breathing, yoga, and meditation have been shown to reduce hot flush frequency and intensity.
Mindfulness involves paying attention to the present moment without judgment, which can help reduce anxiety and improve overall well-being. Relaxation techniques aim to reduce muscle tension and promote a sense of calm, which can help alleviate hot flush symptoms.
Long-Term Management: What Can I Take For Hot Flushes

Managing hot flushes in the long term requires a multifaceted approach that involves lifestyle modifications, ongoing medical follow-up, and a personalized treatment plan. By adopting these strategies, individuals can effectively reduce the severity and frequency of hot flushes, improving their overall well-being.
Lifestyle Modifications, What can i take for hot flushes
Lifestyle modifications play a crucial role in managing hot flushes over the long term. These include:
- Maintaining a healthy weight:Excess weight can contribute to hot flushes, as fat tissue produces estrogen, which can trigger hot flushes.
- Regular exercise:Physical activity helps regulate body temperature and can reduce the frequency and intensity of hot flushes.
- Dietary changes:Avoiding spicy foods, caffeine, and alcohol can help reduce hot flushes, as these substances can trigger vasodilation.
- Stress management techniques:Stress can worsen hot flushes, so it is important to find healthy ways to manage stress, such as yoga, meditation, or deep breathing exercises.
- Cooling techniques:Wearing loose, breathable clothing, using a fan or air conditioning, and taking cool showers or baths can help reduce body temperature and prevent hot flushes.
Ongoing Medical Follow-up
Regular medical follow-up is essential for managing hot flushes in the long term. This allows healthcare providers to monitor the effectiveness of treatment, adjust medications as needed, and address any underlying health conditions that may be contributing to hot flushes.
Conclusive Thoughts
Managing hot flashes requires a multifaceted approach that addresses both physical and emotional well-being. By implementing lifestyle modifications, exploring over-the-counter remedies, and considering prescription medications or alternative therapies as needed, individuals can effectively mitigate the impact of hot flashes on their daily lives.
Remember, you are not alone in this journey. With the right strategies and support, you can regain control and embrace a life free from the discomfort and disruption caused by hot flashes.
Popular Questions
What causes hot flashes?
Hot flashes are primarily caused by hormonal fluctuations, particularly a decrease in estrogen levels during menopause. However, other factors such as certain medications, medical conditions, and lifestyle habits can also trigger hot flashes.
How long do hot flashes typically last?
The duration of hot flashes varies from person to person. On average, they can last anywhere from a few seconds to several minutes, with some individuals experiencing multiple episodes throughout the day.
What are some effective lifestyle modifications for managing hot flashes?
Lifestyle modifications such as maintaining a healthy weight, managing stress, avoiding triggers like caffeine and alcohol, and getting regular exercise can help reduce the frequency and severity of hot flashes.
When should I consider prescription medications for hot flashes?
If lifestyle modifications and over-the-counter remedies do not provide sufficient relief, prescription medications may be an option. Hormone replacement therapy (HRT) and selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to manage hot flashes.
Are there any alternative therapies that can help with hot flashes?
Alternative therapies such as acupuncture, herbal remedies, and relaxation techniques have shown promise in alleviating hot flashes. However, it’s important to consult with a healthcare professional before using any alternative therapies.