What causes hot flashes in females – Delving into the complexities of female physiology, we explore the underlying causes of hot flashes, a common experience during menopause. As hormone levels fluctuate and the body undergoes significant changes, understanding the triggers that ignite these sudden sensations of heat is crucial for managing their impact.
This comprehensive guide delves into the intricate interplay of hormones, neurotransmitters, and the autonomic nervous system, unraveling the mechanisms that contribute to hot flashes. We will also examine lifestyle factors, medical conditions, and treatment options, empowering individuals with knowledge and strategies to navigate this phase of life with confidence.
Neurotransmitters: What Causes Hot Flashes In Females
Neurotransmitters are chemical messengers that transmit signals between nerve cells in the brain and body. In the context of hot flashes, certain neurotransmitters, particularly serotonin and norepinephrine, play a significant role.
Serotonin is a neurotransmitter that is involved in mood regulation, appetite, and sleep. Decreased levels of serotonin have been associated with increased frequency and severity of hot flashes. Norepinephrine is another neurotransmitter that is involved in arousal, attention, and blood pressure regulation.
Imbalances in norepinephrine levels can also contribute to vasomotor symptoms.
Serotonin
- Low serotonin levels have been linked to increased hot flash frequency and severity.
- Serotonin helps regulate body temperature, and decreased levels can disrupt this regulation.
- Certain medications that increase serotonin levels, such as selective serotonin reuptake inhibitors (SSRIs), have been shown to reduce hot flash symptoms.
Norepinephrine
- Norepinephrine is involved in blood pressure regulation and can influence blood flow to the skin.
- Sudden changes in norepinephrine levels can trigger vasodilation, leading to hot flashes.
- Medications that block norepinephrine receptors, such as beta-blockers, have been found to be effective in reducing hot flash severity.
Blood Vessels
Blood vessels play a crucial role in heat dissipation and regulation within the body. They act as a network of channels that transport blood throughout the body, carrying heat away from the core and distributing it to the extremities.
Vasodilation, the widening of blood vessels, increases blood flow to the skin’s surface, promoting heat dissipation. Conversely, vasoconstriction, the narrowing of blood vessels, reduces blood flow to the skin, conserving heat within the body.
Hot Flashes
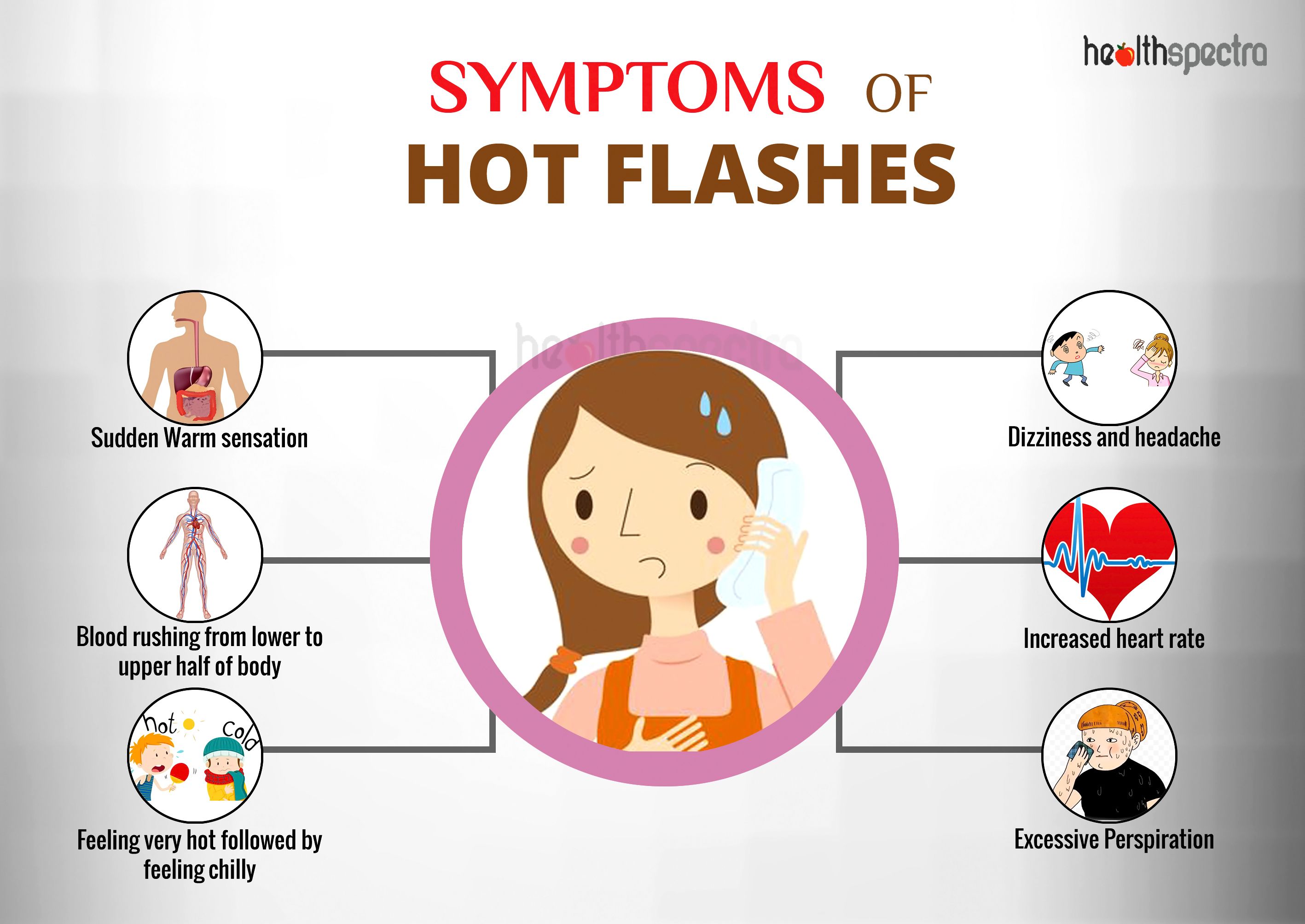
During hot flashes, the body experiences a sudden and intense feeling of heat, often accompanied by sweating and flushing of the skin. This phenomenon is caused by a temporary disruption in the body’s thermoregulatory system.
When a hot flash occurs, the hypothalamus, the brain’s temperature control center, misinterprets a slight increase in body temperature as a sign of overheating. In response, the hypothalamus triggers vasodilation, causing blood vessels near the skin’s surface to widen. This increased blood flow to the skin leads to the characteristic sensations of heat and flushing.
Autonomic Nervous System
The autonomic nervous system (ANS) plays a crucial role in maintaining body temperature through its sympathetic and parasympathetic branches. The sympathetic branch activates heat-producing mechanisms, such as vasoconstriction and increased metabolic rate, while the parasympathetic branch promotes heat loss through vasodilation and sweating.
Disruptions in ANS
Dysregulation of the ANS, particularly involving the sympathetic and parasympathetic branches, can contribute to hot flashes. Overactivity of the sympathetic nervous system may lead to excessive vasoconstriction and increased body temperature, triggering hot flashes. Conversely, underactivity of the parasympathetic nervous system may impair heat dissipation through sweating and vasodilation, exacerbating hot flashes.
Lifestyle Factors
Lifestyle choices can significantly influence the frequency and severity of hot flashes in females. Understanding these factors and making appropriate modifications can help alleviate symptoms and improve overall well-being.
Diet
Certain dietary components can trigger or exacerbate hot flashes. Foods high in sugar, processed ingredients, and unhealthy fats have been linked to increased hot flash frequency. On the other hand, consuming a balanced diet rich in fruits, vegetables, and whole grains can help regulate body temperature and reduce hot flash severity.
Exercise
Regular exercise can improve circulation, regulate body temperature, and reduce stress levels, all of which can contribute to fewer and less intense hot flashes. However, it is important to avoid exercising in extreme heat or humidity, as this can trigger hot flashes.
Stress
Stress is a major contributor to hot flashes. When under stress, the body releases hormones like cortisol and adrenaline, which can cause blood vessels to dilate and increase body temperature. Engaging in stress-reducing activities such as yoga, meditation, or deep breathing exercises can help manage stress levels and reduce hot flash frequency.
Medical Conditions
Certain medical conditions can disrupt the body’s temperature regulation, leading to hot flashes.
One common cause is thyroid disorders, such as hyperthyroidism (overactive thyroid). This condition causes the body to produce excessive thyroid hormones, which can accelerate metabolism and increase body temperature.
Cancer Treatments, What causes hot flashes in females
Some cancer treatments, such as chemotherapy and radiation therapy, can also trigger hot flashes. These treatments may damage the ovaries, leading to a decrease in estrogen production. Estrogen plays a crucial role in regulating body temperature, and its decline can cause hot flashes.
Treatment Options
Hot flashes can be managed through various treatment options, including hormone replacement therapy, medications, and complementary therapies. The choice of treatment depends on individual circumstances, such as the severity of hot flashes, overall health, and personal preferences.
Hormone Replacement Therapy (HRT)
HRT involves taking hormones, typically estrogen or a combination of estrogen and progestin, to supplement the declining levels of these hormones during menopause. HRT can effectively reduce the frequency and severity of hot flashes. However, it may increase the risk of certain health conditions, such as blood clots, stroke, and breast cancer, especially in women with a history of these conditions.
Medications
Non-hormonal medications can also be used to treat hot flashes. These include:
- Selective serotonin reuptake inhibitors (SSRIs), such as paroxetine and venlafaxine, which can help regulate mood and reduce hot flashes.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine and duloxetine, which have similar effects to SSRIs.
- Clonidine, an antihypertensive medication that can reduce the intensity of hot flashes.
Complementary Therapies
Complementary therapies may provide additional support in managing hot flashes. These include:
- Yoga and Tai Chi: These mind-body practices can help reduce stress and improve overall well-being, which may positively impact hot flashes.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to stimulate energy flow. Acupuncture may help reduce the frequency and severity of hot flashes.
- Herbal remedies: Some herbal remedies, such as black cohosh and red clover, may have estrogen-like effects and may help alleviate hot flashes. However, it’s important to consult a healthcare professional before using herbal remedies.
Conclusive Thoughts
In conclusion, hot flashes are a multifaceted experience influenced by a complex interplay of physiological and external factors. Understanding the underlying causes empowers individuals to make informed choices about their health and well-being. By embracing lifestyle modifications, seeking medical advice when necessary, and exploring various treatment options, women can effectively manage hot flashes and maintain a fulfilling quality of life during menopause and beyond.
FAQ
What are the primary hormones involved in hot flashes?
Estrogen and progesterone play crucial roles in regulating body temperature. During menopause, declining estrogen levels can disrupt this regulation, leading to hot flashes.
How do neurotransmitters contribute to hot flashes?
Neurotransmitters such as serotonin and norepinephrine influence vasomotor function. Imbalances in these neurotransmitters can trigger vasodilation, resulting in hot flashes.
What role does the autonomic nervous system play in hot flashes?
The autonomic nervous system controls body temperature. Disruptions in the sympathetic and parasympathetic branches can lead to vasomotor instability, contributing to hot flashes.